|
Subscribe / Renew |
|
|
Contact Us |
|
| ► Subscribe to our Free Weekly Newsletter | |
| home | Welcome, sign in or click here to subscribe. | login |
Construction
| |
 |
June 23, 2011
Group Health is designing its clinic of the future
Group Health Cooperative and GLY Construction

Erikson
|

Elliott
|
What if there was a new way to design and build our medical centers? A way in which clinical staff, leaders, architects and builders worked together from day one to create a facility that truly met patient, staff and business needs for years to come?
Well, that future is here now. Changing the design and delivery of health care facilities involves an investment for decades, so it’s important to get everyone in the room and get it right.
So that’s what we are doing. With several clinics scheduled for replacement in 2012 and beyond, Group Health Cooperative saw an opportunity to design an environment that supports an unparalleled patient experience, and joined with partners CollinsWoerman and GLY Construction to pursue that vision.
Today’s thinking about the future begins and ends with the patient, bringing together all the pieces of the patient experience, both business aspects and care. As it turns out, putting the patient first is also good for health care providers, designers and builders — saving time, money and resources over the long term. The underlying idea is to design patient-care processes, business processes and physical clinic space in parallel with each other.
What does this mean? First and foremost, it means bringing services directly to patients and making their input, time and convenience the top priority. It means leveraging cutting-edge technology and communication systems to streamline delivery and record keeping, and improve clinical outcomes. It means designing layout prototypes and building modular spaces that increase flexibility and efficiency over the long term. It also means designing and building facilities to be more sustainable, using less energy over the life of the building and maximizing healthy conditions for both patients and staff.
Going beyond design
To realize these goals, Group Health, CollinsWoerman and GLY began a process called integrated care and facility design, or ICFD, to plan the clinics of the (near and far) future. Current concepts of lean design, 3P (Production Preparation Process), and integrated project delivery are integral, but ICFD takes them a step beyond project design to incorporate patient care, business process and long-term sustainability.
From GLY’s perspective, the integration of all key team members from the beginning created alignment around a single vision for the future of patient-centered care. We could better understand how Group Health Cooperative operated, how different service lines and departments work together and how the construction team could help build flexibility into the new clinics that would allow patient care to evolve over time. Together, we’ve brainstormed and begun to test the most desirable options to determine their feasibility and opportunities.
From Group Health’s perspective, there was an opportunity to learn how 3P improvements could help standardize a build process that is faster and less costly while being more collaborative and effective. In our case, that process looks at how care and business processes can work differently within a design built for flexible use long into the future, while improving quality and flow of care for the patient.
Because this process offers opportunities for transformational improvements, our target goals are ambitious. They include:
• 80 percent fewer handoffs during the patient-care process.
• 50 percent less distance traveled by patients and staff.
• 50 percent less space used for patient waiting areas and storage.
• 100 percent of the clinical space to be multifunctional to support either primary care or specialty practices.
• No post-project work orders.
• LEED gold certification achieved within 12 months of completion.
“These targets are intentionally high to encourage creative, breakthrough solutions,” Lee Fried of Group Health explains.
“Teams can simply work harder to achieve a 10 percent improvement, while a 50 percent or greater improvement takes a completely different system and level of improvement. Setting stretch goals, if done correctly, can be inspirational and motivating.”
Stretching is probably the only way to get there. The 3P process is aggressive and involves a substantial time commitment from delivery system leaders, clinic staff, and design and construction teams to make it work. And every step needs to be informed by patient research and feedback.
We’re asking patients what works for them, and in the process discovering that improvements such as faster check-in, less waiting, prescription drugs by mail, better communication and access to medical personnel, and streamlined checkout, copay and billing processes segue neatly with streamlined business processes.
Patients also tend to prefer one location for all their health care needs, from well care to specialized and acute care, along with more direct access to their team of providers. So we’re thinking through how to bring all services to them in one place.
First, we must determine “patient flow” through the clinic for various health care needs, to the point of shadowing them. Then we can build that efficient flow into the system, whether in the physical space or cyberspace equivalent.
A place to test ideas
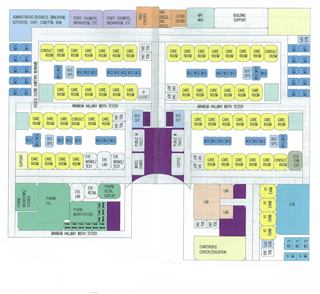
Standardization of clinic processes and flow, regardless of location, allows for standardization of the built environment. This in turn helps us create adaptable, flexible spaces to accommodate future changes of use that can’t really be anticipated today. Using a modular grid for standardization of room sizes also allows maximum future flexibility with minimal changes or disruption inside already occupied and operating clinics.
In addition, we’re planning healthier spaces for long-term viability. Again, the ICFD process is examining the experiences of patients and staff to determine environmental sensitivities and incorporate daylighting, natural screening with trees, locally sourced materials and low-energy consumption.
We are even exploring putting energy back into the grid, with a long-term focus on lower costs over time and higher comfort levels for staff and patients. Our goal is to set a new standard for nonconventional mechanical or electrical systems where long-term performance, compatibility with other materials and components, flexibility, sustainability and life-cycle costs are more important than first costs.
To achieve all of this, we’re developing concepts, diagramming and then mocking up the results in temporary replicas. A leased warehouse will be used over the next year to test ideas, showcase possible design and construction solutions, and run real-time simulations of patient care to see how new concepts will work prior to the start of construction. Patients and representatives from other medical centers will be invited to walk through or virtually visit our full-scale mock-ups and share their insights on proposed designs for work flows and space.
This hard work up front is worth it. The resulting design will provide a prototype for all future clinics, with the ability to be duplicated on multiple sites with minimal time to design and build. The prototype will have flexibility built into it, so we learn from early buildings what to improve in later buildings, and can easily change up to new uses.
It’s a bit daunting since we don’t yet know the final outcome for satisfying all of our goals, yet it’s exciting to think about what we’ll achieve in the next few months — for patients, staff, and for our knowledge of innovations that move boldly into the future of better patient care and outcomes.
Michael Erikson is vice president of primary care services at Group Health Cooperative. Jim Elliott is a principal and health care specialist at GLY Construction.
Other Stories:
- 13 tips for choosing your medical space
- Study will help UW’s Montlake Tower cut energy costs
- Swedish Issaquah aligns design with patient needs
- Good signage points the way to better health care
- 'Novel' process lets Swedish Issaquah hit fast forward
- ‘Hybrid’ rooms a low-cost answer to space needs
- Swedish women’s cancer center a one-stop shop
- Puyallup hospital tower puts focus on patients
- Evergreen opens center closer to its patients
- New VA complex to treat ‘emerging’ war injuries
- Friday Harbor hospital aims to be nation’s greenest
- UW expansion stays on track despite big change in plans